Abstract
Introduction: Immune thrombocytopenia (ITP) is an autoimmune phenomenon causing increased destruction and insufficient platelet production. ITP can be a healthcare burden due to prolonged treatment (medical and sometimes surgical = splenectomy) required to prevent the relapse and frequent hospitalizations for management of complications such as epistaxis, gastrointestinal bleeding (GIB) or intracranial hemorrhage (ICH). In addition, septicemia and coagulation disorders can occur related to therapy. In this study we analyzed demographics among inpatient admissions with ITP and the variation of length of stay (LOS) and mortality with different complications.
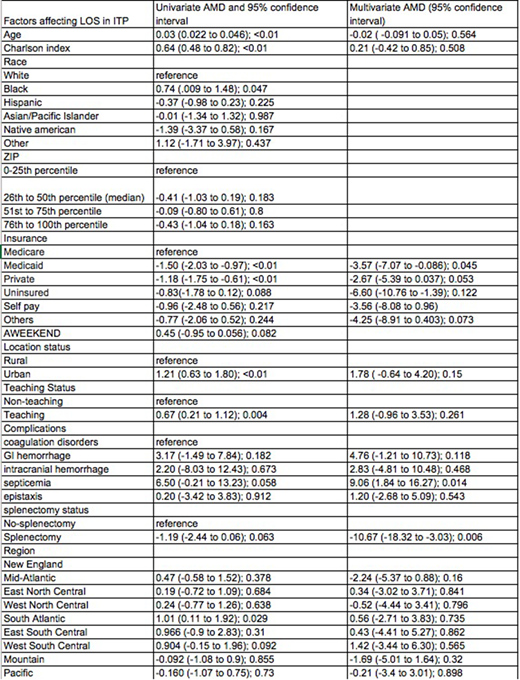
Methods: We performed a retrospective cohort analysis of the National Inpatient Sample 2014 Database (HCUP-NIS). Patients were included in the study if they had a primary or secondary diagnosis of ITP and age >18 years. We performed descriptive statistics to characterize the cohort in terms of personal demographic factors (age, race, sex, insurance type, community level income level), hospital characteristics (size, region, teaching status, and urban or rural location). The cohort was classified on based on splenectomy status using procedure diagnosis code. The cohort was further analyzed for complications such as coagulation disorders, GIB, ICH, septicemia and epistaxis using their principal diagnosis. Furthermore, we also looked at the variation in LOS and mortality among them. Univariate and multivariate regression analysis were performed to determine statistical significance. All analyses applied the HCUP-NIS weights.
Results: There were 11,535 patients in the cohort. Most were white (64.4%), females (57.95%), and aged < 60 years (55.6%). A significant proportion were covered by Medicare (41.33%). Most care was delivered in large hospitals (55.17%), that were disproportionately urban (94.4%) or teaching (70.61%) institutions. The greatest segment of patients were in the South Atlantic region (20.8%). Epistaxis occurred in 15.3% of patients, GIB in 3.12%, ICH in 0.41%, and septicemia in 0.99%. The mean LOS was 4.73 days (95% CI 4.49 to 4.97). Mean LOS was highest in patients with septicemia (12.3 days), followed by GIB (8.98 days) and ICH (7.99 days), and epistaxis and coagulation disorders (6 days each). LOS was significantly shorter in patients who had undergone splenectomy (AMD -10.67 95% CI-18.32 to -3.03), and longer with septicemia (AMD 9.06 95% CI 1.84 to 16.27). Compared to Medicare, other insurances statuses had shower LOS: uninsured (AMD -6.60 95% CI -10.76 to -1.39), Medicaid (AMD -3.57 95% CI -7.07 to -0.086), and private (AMD -2.67 95% CI -5.39 to 0.037). Risk of death was much higher with GIB (OR 227 95% CI 7.63 to 6757.48, p=0.002) and ICH (OR 100.88 95% CI 10.27 to 990.91, p <0.01).
Discussion: Treatment and complications significantly impact LOS and mortality for patients with ITP. Splenectomy is associated with decreased LOS, presumably because of rapid improvement in platelet counts, while septicemia is associated with increased LOS likely related to intensity of service delivered. Insurance types are also independently associated with LOS. It is unclear if this is related to differences in biologic factors (e.g. age, comorbidities, frailty), or process factors (e.g. care management practices, payment incentives).
Bussel:Amgen Inc.: Consultancy, Research Funding; Momenta: Consultancy; Prophylix: Consultancy, Research Funding; Protalex: Consultancy; Uptodate: Honoraria; Rigel: Consultancy, Research Funding; Novartis: Consultancy, Research Funding. Marks:Lilly: Membership on an entity's Board of Directors or advisory committees; UPMC: Employment; Heron: Membership on an entity's Board of Directors or advisory committees; Odonate: Membership on an entity's Board of Directors or advisory committees; Seattle Genetics: Equity Ownership.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal